Your Cycle Phases
Lesson 3
Lesson Objectives:
-
Be able to identify and understand the major events and phases of the menstrual cycle.
-
Build a foundation of knowledge about the menstrual cycle so that fertility charting makes sense.
Major Points in this Lesson:
-
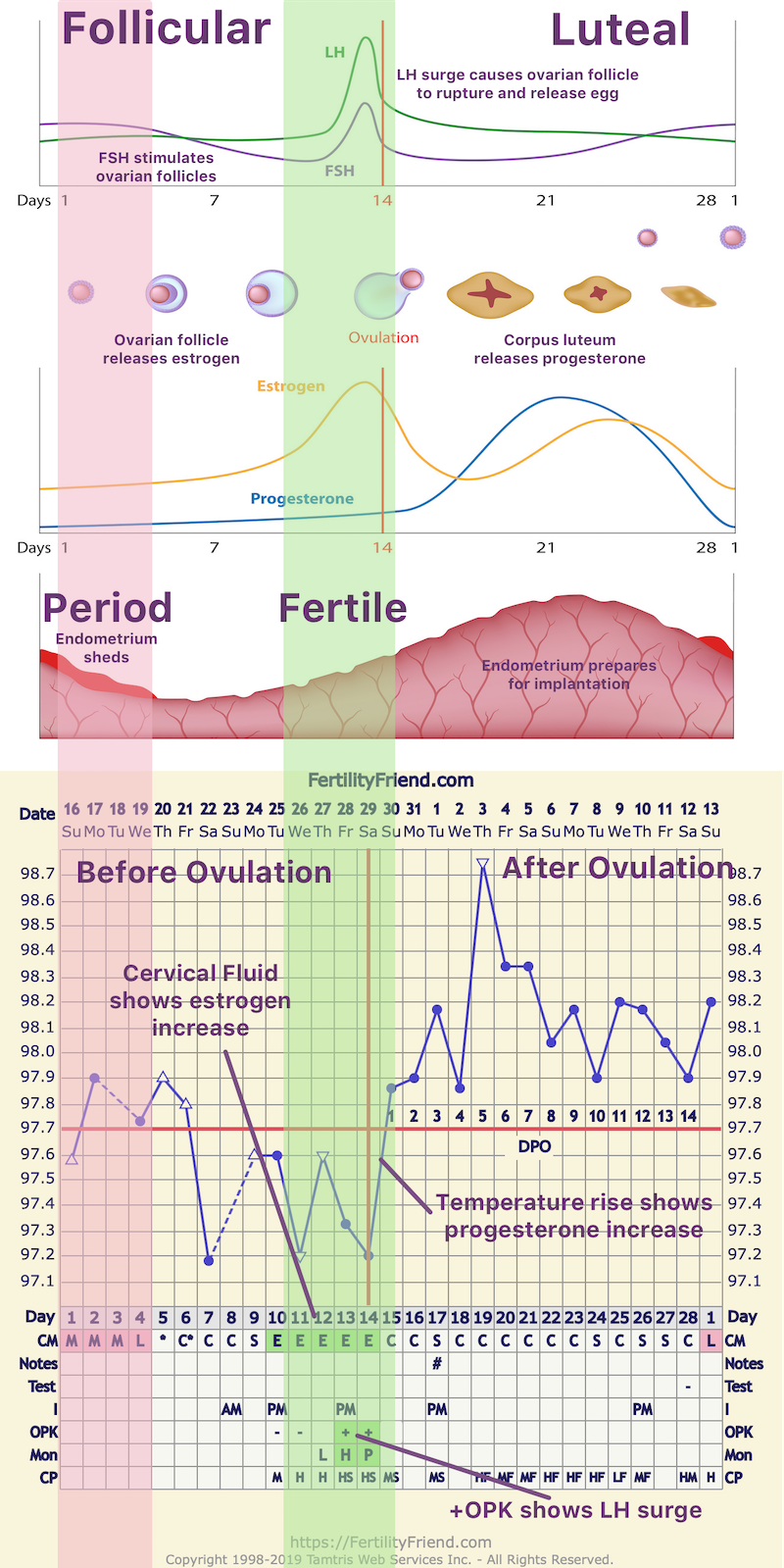
The menstrual cycle can be divided into the following phases: menses, the follicular phase (before ovulation), ovulation, and the luteal phase (after ovulation).
-
Ovulation is the event that divides the follicular and luteal phases.
-
The follicular phase length may vary from cycle to cycle and from woman to woman. It is the follicular phase length that determines the cycle length and cycle length variations.
-
The luteal phase length is constant, rarely changing by more than a day or two from cycle to cycle for the same woman.
-
The luteal phase usually lasts from 12-14 days, but may last from 10-16 days.
-
The best time to conceive is just before and during ovulation .
More...
This lesson, though more complicated than many of the lessons in this course, is included towards the beginning of the course because your fertility signs and your chart will be more meaningful to you when you can correlate them with the significant events and hormonal processes of your menstrual cycle.
Cycle Phases:
Your cycle is composed of the following phases:
-
Menses (M): This is your period. You are generally not fertile at this time.
-
Follicular Phase: The follicular phase extends from the beginning of the cycle until ovulation. During this phase the ovarian follicles develop and mature and your body prepares for ovulation. One follicle becomes dominant as the phase progresses. The length of this phase can vary from woman to woman and from cycle to cycle. You are most fertile at the end of this phase during the days just before and including ovulation. The hormone estrogen dominates this phase.
-
Ovulation: This is the event that divides the follicular and luteal phases. Triggered by a surge of luteinizing hormone (LH), the ovarian follicle ruptures and releases the ovum which can then be fertilized.
-
Luteal Phase (LP): This is the time from ovulation until the end of the cycle. If you conceive, the fertilized egg will implant in your uterine lining roughly 7-10 days into this phase. If there is no conception, the uterine lining will be shed (this is your period) and your body will begin to prepare for a new cycle. This phase usually lasts 12-14 days but can last between 10-16 days. The length of this phase is fairly constant from cycle to cycle for the same woman. Progesterone is the hormone that dominates this phase.
The image below shows the cycle phases along with the corresponding hormonal changes and physiological events. At the bottom of the image, you can see how they can be displayed on a fertility chart:
And more...
What happens during the menstrual cycle phases?
Your menstrual cycle is driven by your hormones. Hormones are biochemical substances that are produced in one area of your body and carried in your bloodstream to send signals that trigger responses in another part of your body. The hormones that control your fertility signals are produced in the following areas:
-
Hypothalamus (in your brain)
-
Anterior pituitary gland (also in your brain, located behind and attached to the hypothalamus)
-
Ovaries
-
Adrenal glands (located on top of your kidneys).
A series of hormonal steps trigger the events of your menstrual cycle:
-
At the beginning of your menstrual cycle, the hypothalamus produces GnRH (gonadotropin-releasing hormone). The GnRH pulses through your bloodstream from the hypothalamus to the pituitary gland in spurts every 60-90 minutes from menstruation until ovulation. The GnRH signals the anterior pituitary gland to secrete FSH (Follicle Stimulating Hormone) and later LH (Luteinizing Hormone). This is what is happening when you have your period and in the days before ovulation.
-
The Follicle Stimulating Hormone (FSH), as its name suggests, stimulates the development and maturation of follicles in the ovaries. One of these follicles will become dominant and contains the ovum that will be released at ovulation. The developing follicles begin to produce estrogen.
-
The estrogen released by the developing follicles, and later by the dominant follicle, causes the lining of the uterus, the endometrium, to grow and thicken in preparation of implantation of a fertilized ovum.
-
By about the seventh day of your cycle on average (but this can vary widely) the dominant follicle takes over. The eggs within the other follicles lose their nourishment and die as do the follicular cells.
-
The dominant follicle produces a sharp rise in estrogen. (You can recognize this stage of your cycle by closely monitoring your cervical fluid). Estrogen is at its peak one to two days prior to ovulation.
-
This estrogen surge signals the release of LH (Luteinizing Hormone). This is the hormone that is measured by ovulation predictor kits (OPKs). LH travels through the bloodstream to the ovary where it causes the ovary to release enzymes that make a hole in the sac of the dominant follicle. This causes the dominant follicle to rupture and release the ovum into the fallopian tube where it can be fertilized. This is ovulation. The LH surge is necessary for ovulation to occur. The LH surge (the highest concentration of LH) occurs 12-24 hours prior to ovulation but LH begins to rise about 36 hours before ovulation.
-
Estrogen drops dramatically after ovulation.
-
The dominant follicle, transformed by LH, becomes the corpus luteum after ovulation. This phase of your cycle after ovulation is called the luteal phase since hormone production is governed by the corpus luteum. The corpus luteum continues to produce a small amount estrogen, but now also produces progesterone. Progesterone is the hormone that dominates this phase of your cycle. Like estrogen, progesterone is needed to develop the endometrium so that a fertilized egg can implant and be nourished should fertilization occur. Your BBT (Basal Body Temperature) rises as a result of progesterone production.
-
If an egg is fertilized and implantation of the fertilized egg occurs, the corpus luteum's life is extended. In conception cycles, the corpus luteum keeps on producing progesterone and some estrogen and the development of the endometrium continues. The pregnancy hormone, hCG begins to be produced when the fertilized egg implants, at around 7-10 days past ovulation. As the pregnancy progresses, hormone production is taken over by the placenta.
-
If there is no pregnancy, the corpus luteum dies, progesterone levels fall, and a new cycle begins.
Next Lesson: Your Hormones and Your Fertility Signals
Note: Please check this lesson within the app to access the lesson quiz.

